New study explores whether depression could increase risk of MS progression
Several previous studies suggested experiencing depression when you have MS, could be linked to increased disability later on. But a new paper from the UK MS Register hasn’t found any evidence to support that.
We know depression is common in people with MS. Studies in Canada and Sweden looked at people living with MS and depression. And found they could be more likely to reach disability milestones than people without depression.
But a UK study published today suggests depression may be a result of more advanced disability, rather than a cause.
The researchers found what appeared to be a link between early depression and going on to reach a higher level of disability. But this link disappeared when they took into account people’s earlier level of disability.
Read about the Canadian study on the journal website
Read about the Swedish Study on the journal website
What did the researchers do?
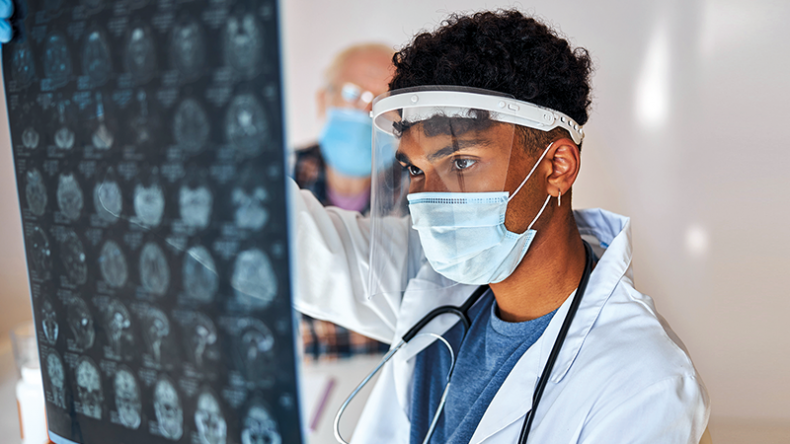
In July 2022, the UK MS Register ran a ‘datathon’ event. This was to help MS researchers in the early stages of their careers learn how to use big datasets to answer questions about MS.
A team from Swansea University, University of Cambridge and Queen Mary University of London won a prize for doing the best analysis. And now they’ve published their results.
They analysed data from 862 people with MS using information from the UK MS Register. Everyone completed a questionnaire called the Hospital Anxiety and Depression Scale (HADS). The researchers considered a score of 8 or above to mean someone was experiencing anxiety or depression.
They combined this with people’s Expanded Disability Status Scale (EDSS) scores. They looked at whether people reached an EDSS score of 6.0. This means you need a walking aid to walk about 100 metres with or without resting.
What did they find?
Over a third (43.3%) of people who progressed to a score of 6.0 on the EDSS reported feeling depressed early in their MS journey. This was compared to less than a quarter (22.4%) of people who didn't reach 6.0.
Importantly though, this difference was lost when the researchers took into account people’s initial level of disability. So rather than depression impacting disability worsening, they suggest their results are likely to be showing the big challenges of living with MS. Greater disability can cause people to feel more depressed.
But they do acknowledge there could be other explanations for their results. For example, there could be a common factor increasing the risk of both disability and depression, such as more brain lesions.
What do these results mean?
More than a quarter (25.6%) of people in the study had high depression scores. And more than 40% had high anxiety scores.
Dr Benjamin Jacobs, one of the co-authors on the study, says “Our study shows that depression is common in MS, particularly in people who have a more disabling course. Recognising and treating depression in MS is unlikely to affect the disease itself, but may have an important positive impact on quality of life.”
Dr Emma Gray, our Assistant Director of Research, says “MS can be relentless and painful. And depression affects around half of all people with the condition at some time. Learning that experiencing depression may not cause someone’s MS to get worse will be reassuring for some people. Depression in people with MS cannot be ignored. And knowing high levels of disability might have a major impact on mental health is further evidence.
“This research strengthens the case for prioritising mental health support. And we’ve committed to raise funds for COMPASS-MS. This study will assess a new therapist-supported digital programme to treat distress in MS. It has the potential to help people with MS across the UK who are experiencing symptoms of anxiety and depression.”