What are social determinants of health?
Everyone’s experience of MS is different. People have different symptoms. Some have more relapses or their MS progresses faster. Recent research suggests these differences are influenced by more things than we thought.
We don’t fully understand why everyone’s MS is different. But we do know that how someone’s MS behaves, and the impact this has on them, can be affected by many things, including:
- disease modifying therapies (DMTs)
- other health conditions
- lifestyle, especially smoking
- genetics
Other factors are also important across health and illness. These factors shape how we experience the world, and they influence lots of different conditions.
Social determinants of health
Because they’re relevant to everyone, we call these factors “social determinants of health”. They include:
- Sexuality
- Ethnicity
- Education
- Employment
- Ability to access food and social support
These don’t always stay the same and are often impacted by external forces, which individual people might not have much control over. For example, COVID-19 had a big influence on employment and social networks. And new factors are emerging, like confidence using digital systems.
Research shows we can improve health by influencing some of these circumstances, but we don’t yet know exactly how they impact MS.
Social factors and MS
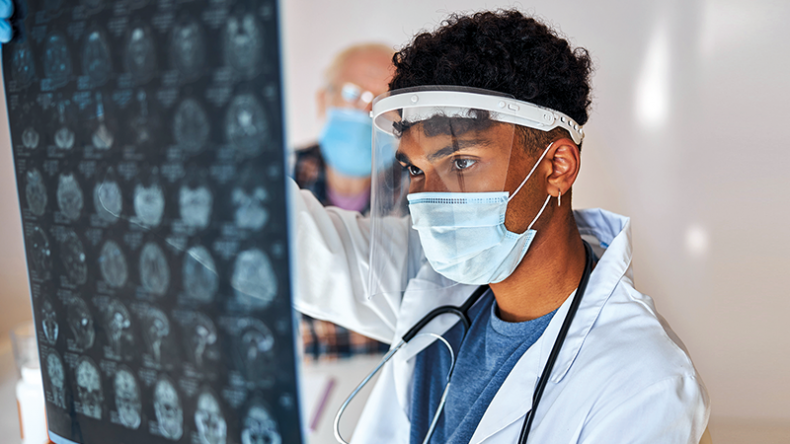
Dr Ruth Dobson and her colleagues recently published a new paper exploring the evidence in MS so far. They believe social factors could play a major role.
There are also factors where there’s been no research in MS. For example, more and more households in the UK are struggling with food poverty, but no studies have examined the effect on MS.
It’s also hard to untangle their separate effects. Lots of them are closely linked and having MS can also affect some factors.
Improving health
We think many social determinants have at least part of their effect through changing how people experience healthcare, rather than through direct effects on MS. That doesn’t make it any less important to tackle these where possible.
Being aware of each person’s circumstances is likely to improve care. So we need to help neurology teams recognise people who have social factors that might make their MS and quality of life worse.
If we address some of these factors, alongside using DMTs and symptom management therapies, we could make living with MS easier. We’ve seen this in other health conditions, but urgently need research to help us understand how to do it in MS.
This blog came from an article in our MS Matters magazine. You can explore the full back catalogue of the magazine.